How Fasting Helps Breast Cancer Treatment Work Better: The Science Behind a Simple Idea
Posted 2 months ago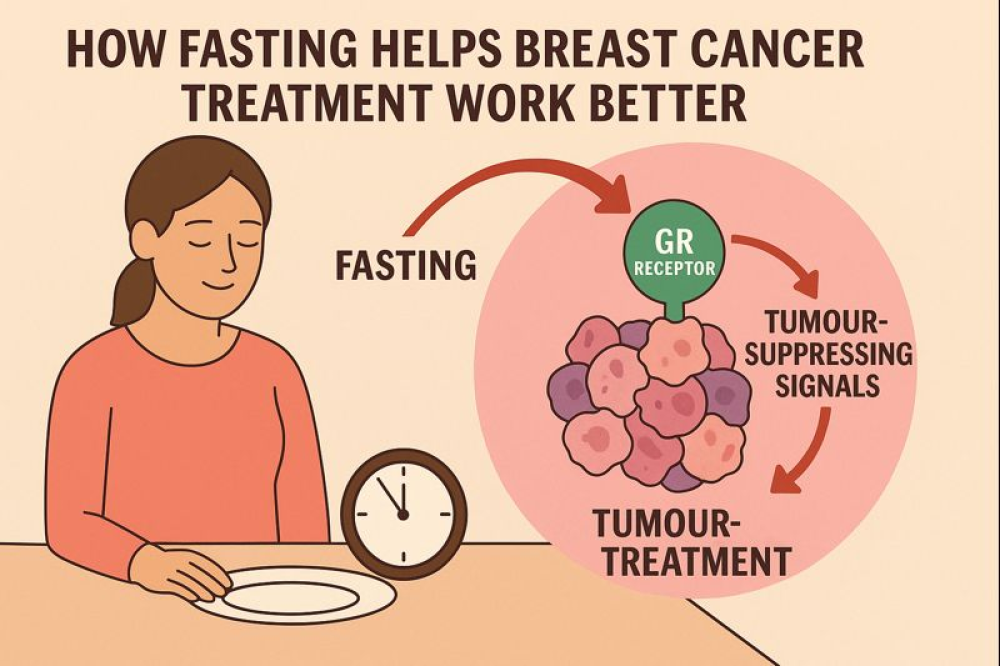
Over the past few years, scientists have been exploring an intriguing idea: can fasting make breast cancer treatments work better? A new study published in Nature provides one of the most straightforward explanations to date, which may inspire confidence in future therapies. The researchers focused on the most common form of breast cancer, hormone-receptor-positive breast cancer (HR+), which relies on hormones like estrogen to grow. These cancers are usually treated with drugs that block hormone signals. At first, the drugs work well, but over time, many tumours learn to escape their effects, leading to treatment resistance. Earlier studies had shown that periodic fasting or fasting-mimicking diets could slow this resistance, but no one fully understood why. This new research fills in the missing pieces, offering hope for improved treatment strategies.
To uncover what fasting really does inside a tumour, the scientists conducted careful experiments using a mouse model implanted with human breast cancer cells. Following the scientific protocol, the First group received the standard treatment drug, the second group followed a controlled 48-hour fasting regimen each week, and the third group received both. The idea was to watch how fasting changed the behaviour of cancer cells at the deepest biological level. They analysed which genes became active or inactive, how deoxyribonucleic acid (DNA) was chemically marked, and which molecular switches controlled the cells. They also compared their findings with data from real breast cancer patients who had followed a specially designed fasting-mimicking diet.
What scientific team discovered was far more sophisticated than simply “starving” a tumour. Fasting caused sweeping changes in how cancer DNA is regulated, a phenomenon scientists call epigenetic reprogramming. These changes switched on a receptor inside cells known as the glucocorticoid receptor, or GR. At the same time, another receptor, the progesterone receptor, also became more active. These receptors triggered a set of genes that slowed cancer growth.
Meanwhile, the fasting group silenced another molecular pathway, Activator Protein (AP-1), which usually drives cancer cell proliferation. In simple words, fasting flips a biological switch that weakens the cancer’s growth signals and strengthens the body’s natural tumour-controlling mechanisms. The researchers also demonstrated the importance of this switch: when they removed the glucocorticoid GR receptor from the cancer cells, fasting no longer provided any benefit. This showed conclusively that GR is a key player in the fasting-related improvement of breast cancer therapy.
The findings may also explain why some patients in earlier small trials showed positive metabolic and hormonal changes after following fasting-mimicking diets. Those diets appeared to activate the same GR-related pathways the researchers saw in mice. While this does not yet prove that fasting alone will cure breast cancer, it strongly suggests that controlled fasting or fasting-like diets can make existing treatments more effective.
The most exciting idea to emerge from this study is that fasting is not the only way to trigger these beneficial biological changes. Since GR is already known to be a receptor activated by common corticosteroid drugs, doctors may one day be able to mimic the benefits of fasting with widely available medicines. This could make treatment easier for patients who cannot fast because of age, weakness, diabetes, or other medical conditions. It may also help doctors design new combination therapies—pairing standard breast cancer drugs with GR-activating medicines to delay resistance and improve long-term outcomes.
These research findings are still at an early stage, and most of the key experiments were conducted in animal models. Continued clinical research is essential to confirm these results and develop new treatments. More studies are needed before fasting or GR-based treatments can become standard medical practice. But the discoveries offer a powerful scientific explanation for why fasting helps hormone therapy work better, and they open a promising new chapter in breast cancer treatment. Instead of relying only on drugs that block hormones, doctors may soon be able to guide cancer cells into a weaker, more vulnerable state—simply by tapping into the body’s natural fasting response, which could lead to more effective therapies in the future.